Workflows and Functionalities
openIMIS is custom built to manage the high-volume data flows which are required to administer health insurance and social protection schemes. It has been specially designed to manage beneficiaries; benefit packages; providers; claims generation, review and processing; payments; and data analysis.
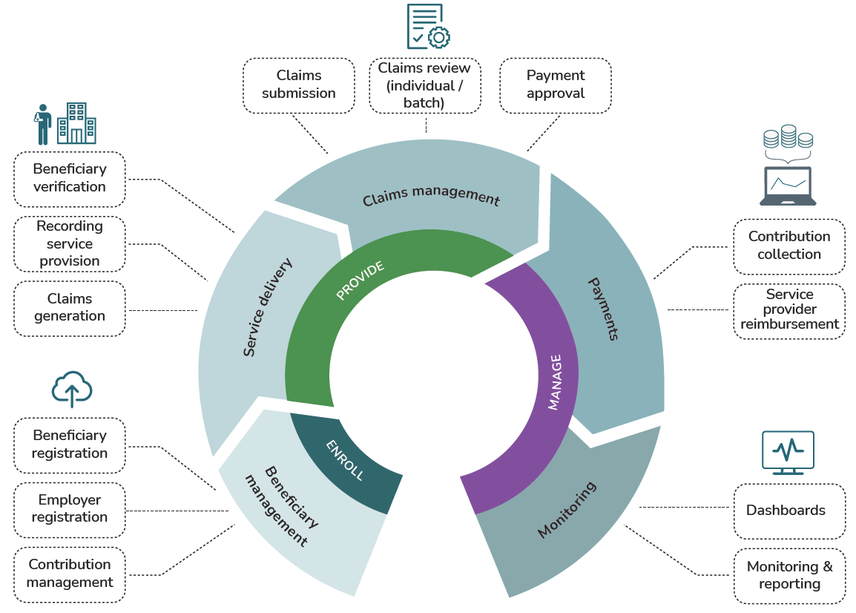
This figure shows one way in which different modules in openIMIS can be used together to manage a particular workflow in social protection schemes. The modular architecture of openIMIS allows the system to be configured and customized in multiple ways to support various workflows.
Beneficiary management
openIMIS supports the enrollment of individuals and families, as well as employers and employees, into schemes. Enrollment information can be captured directly in openIMIS, or imported into openIMIS from existing beneficiary management systems using shared interoperability standards (i.e. HL7 FHIR).
The software supports the renewal of coverage at designated intervals, the updating of beneficiary records and the issuing of ID cards using QR codes and unique identifiers. Enrollment and renewal data, including photos of beneficiaries, can be collected and transmitted using a mobile app.
openIMIS also supports the collection and management of contributions, including issuing payment receipts and tracking whether beneficiary contributions are up to date.
Service delivery
openIMIS supports the verification of scheme membership. When beneficiaries present their ID cards at health facilities, healthcare workers can check their eligibility for services via openIMIS. Beneficiaries are examined and treated, and provided with tests and medicines as needed. The services provided are recorded in openIMIS. Using the software, health facilities can generate claims for insurance scheme operators by entering codes for diagnosis and services rendered.
Claims management
openIMIS supports the submission and review of claims. Health facilities which use openIMIS can electronically submit claims to insurance scheme operators for review. Claims can be processed either individually or in batches. openIMIS allows for claims which pass automated checks (based on pre-defined criteria) to be selected for medical review. It then calculates reimbursements to healthcare providers for approved claims.
Payments
openIMIS supports the management of payments to service providers and to beneficiaries of cash transfer schemes. The payer or scheme operator can use openIMIS to define the criteria for cash transfers (e.g. inclusion criteria, payment amount, frequency) and to generate a payroll with the amounts to be disbursed to beneficiaries in a given payment cycle. Payment service providers use this list to disburse funds. openIMIS also allows for reconciliation of issued payments against payroll. Unique payment transaction numbers can be generated for each payment, allowing them to be traced to individual households.
Monitoring
openIMIS allows scheme operators to monitor and analyse the performance of the scheme through the generation of reports and data visualization, e.g. dashboards.