Health Insurance
The health insurance solution, powered by openIMIS
openIMIS offers a range of functional modules which can be combined into tailored solutions for the delivery of specific social protection schemes. The health insurance solution powered by openIMIS allows scheme operators to manage beneficiaries, contracts, products, contributions, providers, claims and accounting in a single software. A key strength of openIMIS is its capacity to support the digital creation, submission and review of claims, including AI-supported review. It also connects seamlessly with other open source products, such as DHIS2 and openMRS, using FHIR standards.
Supported processes
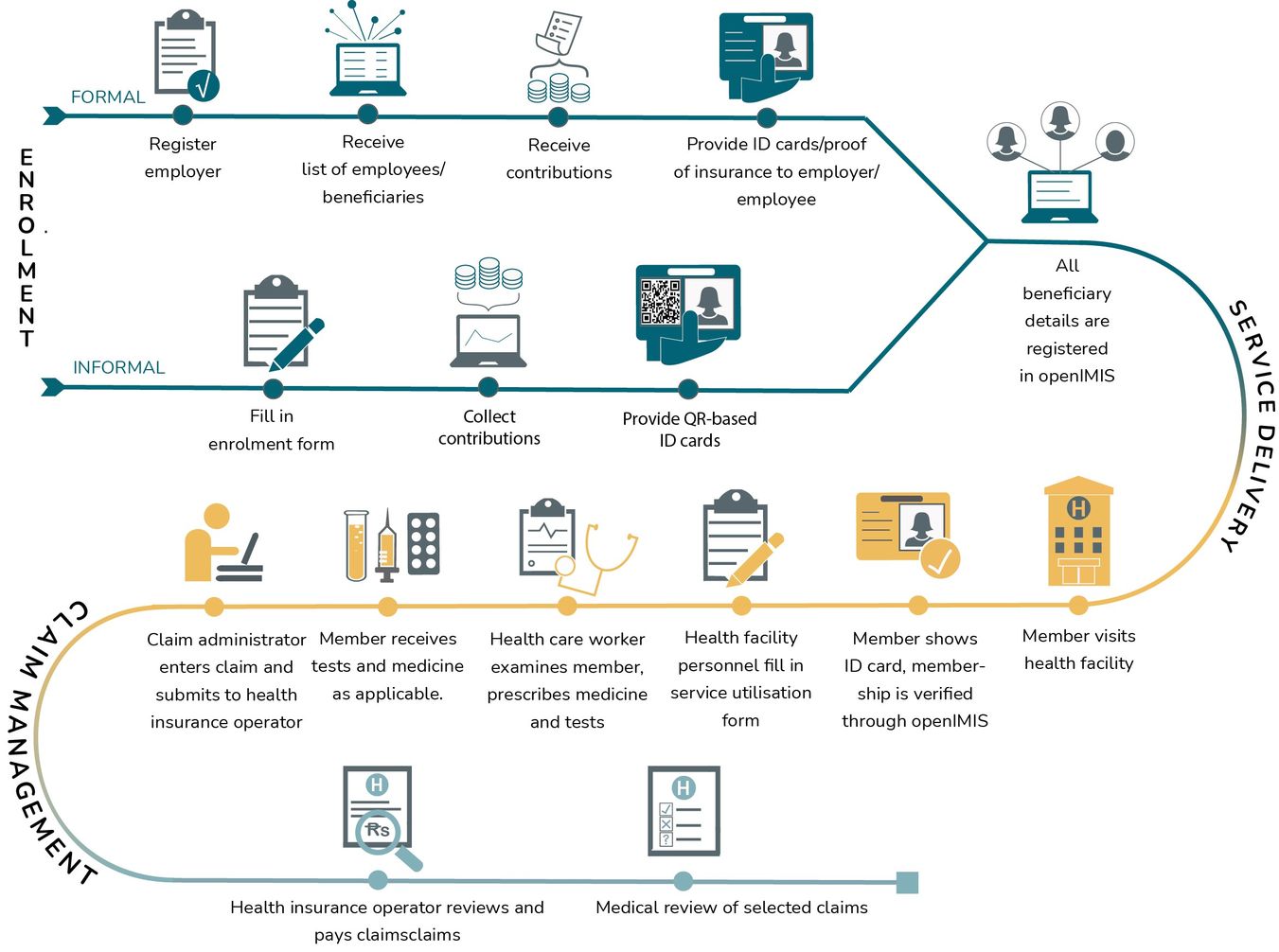
openIMIS supports the following processes for health insurance:
- Employer/employee management
- Collecting and managing contributions
- Benefit package design/configuration
- Issuing membership ID cards to beneficiaries
- Verifying scheme membership
- Health service claims generation and submission
- Claims review and management
- Processing and payment of claims
Benefits
For beneficiaries, openIMIS simplifies enrollment procedures, reduces the number of ‘touch points’ (therefore saving both time and money), and makes it easy to verify one’s coverage status at point of care. For health facilities, it streamlines the processes associated with a health financing scheme and makes it easy for them to receive reimbursements. For scheme operators it reduces operational costs and allows for better monitoring and analysis of the scheme’s overall performance. For decision makers, data from openIMIS can enhance policy making and planning related to health service delivery.
Example workflow
Current implementations
Further information
Visit the wiki page or download the factsheet for the health insurance solution: